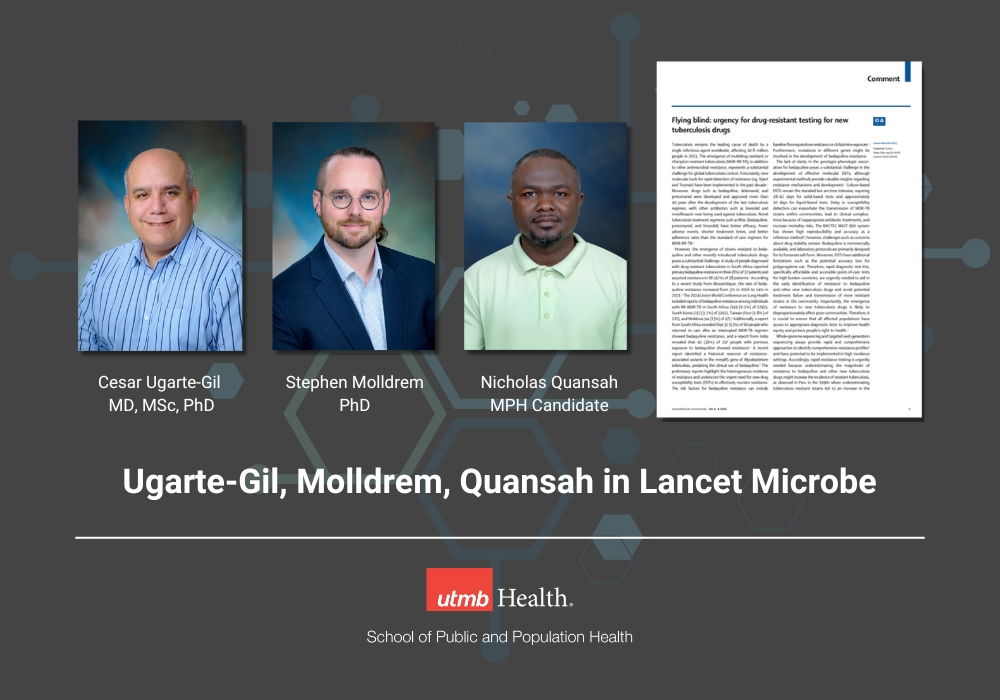
A new commentary in The Lancet Microbe featuring Dr. César Ugarte-Gil, Dr. Stephen Molldrem, and MPH student Nicholas Quansah from the UTMB School of Public and Population Health (SPPH) discusses the concerning spread of drug-resistant tuberculosis (TB). With TB remaining the leading cause of death from a single infectious agent, the emergence of resistance to newly developed treatments—particularly bedaquiline-resistant strains—creates serious worldwide health challenges.
The authors highlight the critical need for improved rapid diagnostic testing, molecular surveillance, and equitable access to drug susceptibility testing (DSTs) to prevent the continued spread of multidrug-resistant and extensively drug-resistant TB (MDR/XDR-TB). Their work helps improve how we fight TB globally, particularly in resource-limited settings where TB hits vulnerable communities hardest.
The Growing Threat of Drug-Resistant Tuberculosis
According to the World Health Organization (WHO), 10.8 million people were diagnosed with TB in 2023, with MDR/XDR-TB cases rising due to incomplete treatments, limited drug access, and delayed diagnosis. The new commentary discusses how mutations leading to bedaquiline resistance have emerged worldwide, undermining a treatment once seen as a breakthrough for drug-resistant TB.
Dr. César Ugarte-Gil, Associate Professor at UTMB SPPH and an expert in TB epidemiology, emphasized the urgent need for drug susceptibility testing (DST) to prevent the rapid loss of new TB treatments before they can have their full impact.
This is especially critical as new regimens like BPaL are being implemented rapidly worldwide. Without robust surveillance, these breakthrough treatments risk becoming ineffective quickly. Strengthening diagnostic capacity must happen alongside new drug deployment to preserve these vital treatment options.
The Role of Genomic Surveillance in Combatting TB Resistance
One of the key solutions proposed in the commentary is the use of whole-genome sequencing (WGS) and targeted next-generation sequencing (tNGS) to rapidly identify drug-resistant TB strains. These technologies allow rapid monitoring of resistance patterns, potentially helping clinicians make faster, more informed treatment decisions while also improving surveillance reporting and prevention outreach.
Dr. Stephen Molldrem, Assistant Professor in Bioethics and Health Humanities at UTMB SPPH, explores the ethical and policy implications of using these genetic tools in TB surveillance programs.
“When ethically implemented with adequate resources and stakeholder engagement, genomic sequencing technologies are powerful tools that can be mobilized to support the identification of drug-resistant TB,” said Dr. Molldrem.
“Given the WHO’s recent recommendation to implement targeted next-generation sequencing for TB in all countries with capacity, it is more important than ever that countries and funders prepare for implementation in ways that ensure access to these innovative diagnostics while respecting the rights of patients, marginalized communities, and all other stakeholders.”
Training the Next Generation of Public Health Experts
Nicholas Quansah, an MPH student focusing on epidemiology, played a key role in this commentary, demonstrating SPPH’s dedication to student involvement in the important discussions in global health problems. His work reflects UTMB’s commitment to training future public health leaders who can apply research findings to real-world global health challenges. He is working now with Dr. Ugarte-Gil on the effects of adverse events in TB patients who are taking bedaquiline.
“Active surveillance will help to clarify the extent of strains resistant to bedaquiline and other new tuberculosis drugs within communities to safeguard the public, maintain the efficacy of new tuberculosis drugs, and improve health outcomes for individuals affected by tuberculosis,” said Quansah.
“Addressing multidrug resistant tuberculosis and antimicrobial resistance requires urgent action, as our survival hinges on how effectively we combat this growing threat. My involvement in this project has deepened my interest in this critical area of public health.”
Why This Research Matters Now
Dr. Neil Mehta, PhD, MSc, MA, Associate Dean for Research at SPPH, highlights the importance of sustained research funding to stay ahead of drug-resistant TB threats. Without continuous investment in surveillance, treatment innovation, and rapid diagnostics, public health risks will continue to escalate globally.
“This commentary makes cogent arguments for why continued investments in TB research is needed even in the face of new and emerging pathogens,” said Dr. Mehta. “The work is an example of UTMB SPPH's emphasis on multidisciplinary collaborations to address pressing public health challenges.”
A Call to Action: Strengthening TB Control Measures
The commentary stresses that rapid resistance testing must become a global standard to prevent further outbreaks of drug-resistant TB. The authors advocate for:
- Scaling up access to next-generation sequencing for early TB resistance detection.
- Developing affordable, accessible point-of-care diagnostics for low-resource settings.
- Implementing stronger policies to ensure equitable treatment access for vulnerable populations.
The study serves as a critical wake-up call for global health leaders to take decisive action on growing TB resistance.
For more information about this commentary, please visit The Lancet Microbe.
Read more about TB in this Ask the Expert article published on World TB Day 2025.
Have news or an event to share? We’d love to feature it on the SPPH News & Events blog! Email SPPHmarketing@utmb.edu with your story ideas.